Washington University School of Medicine in St. Louis and its affiliated hospitals — Barnes-Jewish Hospital and St. Louis Children’s Hospital — are members of Washington University Medical Center, one of the country’s foremost academic medical centers.
Washington University School of Medicine in St. Louis

The medical school has well over a century of success in research, teaching and patient care. It pioneered bedside teaching and has held from the beginning that “investigation and practice are one in spirit, method and object.”
That principle remains in effect today, with the recognition that a good doctor must be a good scientist as well as a compassionate and understanding human being. The school remains a leading institution of clinical care, education and research, ranked annually among the top medical schools in the nation by U.S. News & World Report.
Barnes-Jewish Hospital

Barnes-Jewish Hospital, a 1,346-licensed-bed patient care, teaching and research facility, is the largest hospital in the St. Louis area. Its medical staff is composed exclusively of members of the faculty of Washington University School of Medicine in St. Louis. Consistently listed among America’s elite medical centers in U.S. News & World Report’s list of “America’s Best Hospitals,” BJH has a premier reputation in patient care, medical education, research and community service.
The hospital is a member of BJC HealthCare, the largest academically linked full-spectrum health system in the country. BJC provides community-based and academic health care services at more than 100 inpatient and ambulatory care sites throughout Missouri and southern Illinois.
BJH and the medical school are committed to the management of all aspects of liver disease, including transplantation. In August 1985, the hospital began what was then the 16th liver transplant program in the world. In 1996, Washington University transplant surgeons performed the first adult-to-adult living donor liver transplant in the United States.
BJH and Washington University have always been leaders in the treatment of patients with kidney failure, taking a team approach that includes nephrologists, surgeons, transplant surgeons and nurse coordinators.
The first kidney transplant was performed in 1963, and the first live donor transplant was performed in 1965. In 1968, the hospital became one of the first in the nation to offer hemodialysis and, in 1979, was the third to make available continuous ambulatory peritoneal dialysis (CAPD). The first living-unrelated donor kidney transplant was performed in 1983.
St. Louis Children’s Hospital

St. Louis Children’s Hospital (SLCH) is one of the foremost pediatric hospitals in the country. It provides a full range of health services for children and their families throughout its 200-mile service area and beyond. SLCH also is a member of BJH HealthCare.
Children receive liver transplants at SLCH for liver diseases and congenital defects, most commonly biliary atresia, a bile duct abnormality. Other metabolic disorders that were once fatal can now be corrected through liver transplantation. Refinements in candidate selection and surgical techniques have led to improved outcomes, and the liver program has a high percentage of patients transplanted within the first year of listing. The extensive experience in performing complex liver transplants provides a depth of expertise resulting in outcomes above the national average.
Surgeons at the medical school have the skill and experience to reduce larger livers for use in infants. In 1996, they performed St. Louis’ first split-liver transplant by dividing a donor liver between two recipients.
SLCH was a pioneer in pediatric kidney transplantation, performing its first such operation in 1964. Washington University physicians stress early intervention to minimize complications, and they have successful experience with transplant patients under one year of age.
A multidisciplinary approach characterizes the SLCH kidney transplant program, involving representatives from nephrology, infectious disease, endocrinology, psychology and social services, with oversight by a transplant coordinator.
Mid-America Transplant Center
Mid-America Transplant facilitates the organ and tissue donation process for a service area of 4.7 million people in eastern Missouri, southern Illinois and northeast Arkansas. Mid-America Transplant is the first organ procurement organization in the nation to develop an in-house operating room model for organ recovery, an effort led by Washington University transplant surgeons and reported on in the American Journal of Transplantation.
Institute for Surgical Education (WISE) Center
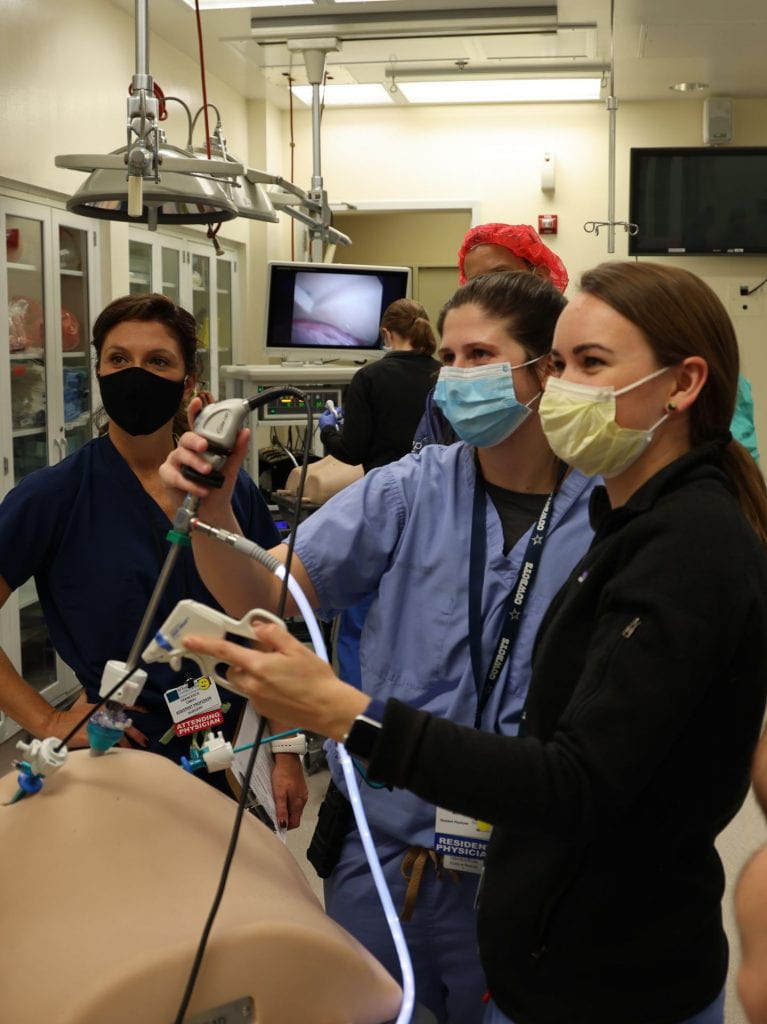
The Washington University Institute for Surgical Education (WISE) Center was one of the first surgical skills labs in the country established to serve a general surgery residency program and continues to train practicing surgeons, all surgical trainees, physicians from other disciplines, medical students, and nurses.
The simulation center has a broad curriculum that includes the use of endoscopy and laparoscopic simulators, training in surgical techniques and instrumentation, cadaver dissection, instruction in emergent procedures and preparation for performing specific surgical procedures. Learn more about the opportunities at WISE.
